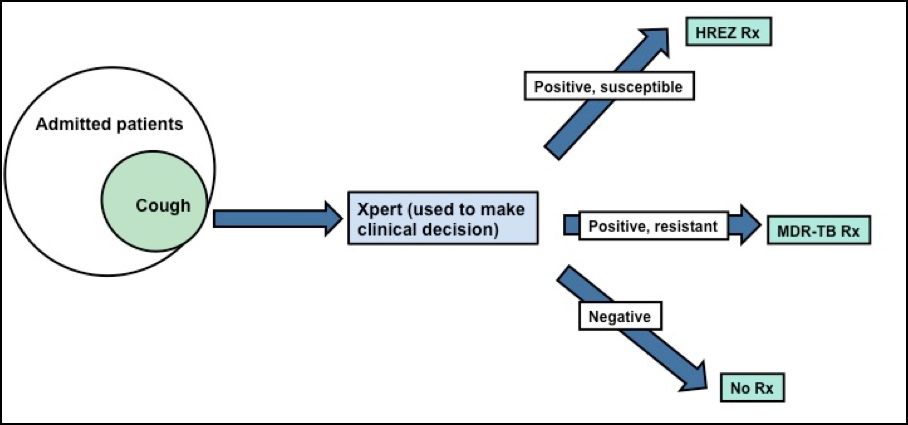
FAST (Find cases Actively, Separate temporarily and Treat effectively) is an intensified, refocused administrative approach to TB transmission control in healthcare facilities. FAST uses active case finding with cough screening followed by rapid molecular diagnostics, which enables prompt treatment of unsuspected drug-sensitive and drug-resistant TB, thereby decreasing TB transmission.
Isn’t FAST simply good clinical care/best practice?
Although evidence-based guidelines on TB-specific infection control (TB-IC) exist, these are often not implemented and health facilities in TB endemic countries often lack TB-IC programs. Additionally, TB-IC practice has traditionally focused on patients with known and suspected TB, whereas evidence demonstrates that transmission is not from known TB patients on effective treatment but rather from patients with unsuspected TB. Under FAST, unsuspected TB patients can be diagnosed and started on effective therapy earlier, thereby decreasing transmission risk.
What is the evidence for FAST?
FAST has been implemented in chest hospitals in Bangladesh, Russia and Vietnam. At all three sites, FAST demonstrated an increase in the number of unsuspected TB and MDR-TB cases identified and a decrease in the time to initiation of effective therapy. In Russia, follow up data since FAST was implemented in 2013 demonstrates lower rates of MDR-TB, suggesting that FAST may be contributing to a decrease in TB transmission.
We are currently in the early years of an NIH-funded dissemination and implementation grant to implement FAST in a large general hospital in Lima, Peru. Enrollment began in August, 2015 and outcomes to be measured will include both the impact of FAST on health care worker TB infection rates, as well as the qualitative aspects of FAST implementation itself. This is the first instance of FAST implementation in a general hospital and will serve to inform similar efforts in other countries.
How can FAST be measured?
FAST implementation can be measured using process indicators such as time from admission to cough detection, time from cough detection to sputum submission, Xpert turnaround time, and time from admission to effective treatment. The impact of FAST on TB transmission can be measured through health care worker TB infection conversion rates.
What are the barriers to FAST implementation?
FAST is feasible and effective but is resource intensive. A dedicated team is required to perform cough surveillance, ensure prompt collection and transport of sputum specimens to the lab, deliver results without delay and ensure that effective treatment is started immediately. Although there are clear individual and public health benefits, ensuring adequate human and material resources as well as the political and financial commitment required to sustain an administrative TB-IC intervention such as FAST over time is challenging.
Grants
Finding and Treating Unsuspected and Resistant TB to Reduce Hospital Transmission